Paxlovid in the Wild Redux
Tagged:COVID
/
JournalClub
/
Math
/
PharmaAndBiotech
What do we know about the people for whom paxlovid works really well?
How Paxlovid Works
We previously wrote a bit on this Crummy Little Blog That Nobody Reads (CLBTNR) about the paxlovid mechansim of action last January, discussing the med-chem optimization of paxlovid. [1]
SARS-CoV2 has a very funny gene called ORF1ab.
- What’s “funny” about it is that it violates the “central dogma” of genetics: one gene makes one protein.
- ORF1ab is a polyprotein gene: it makes a huge string of mRNA, which is transcribed into a huge mess of amino acids that make not much sense as a protien.
- But then another SARS-CoV2 protein called either 3CLpro (“3C-like-protease”) or Mpro (“main protease”) comes along and snips that polyprotein into pieces, some of which fold up into workable proteins.
Yes, biology is a kluge. Surely you are not surprised? Evolution places no premium on elegance by the standards of human understanding.
Paxlovid contains one ingredient called nirmatrelvir that inhibits 3CLpro/Mpro. This has 2 salutary effects:
- The product of ORF1ab is not cloven, remains non-functional, and the virus cannot reproduce.
- There is no homolog of 3CLpro/Mpro in human, so nirmatrelvir can be dosed nice & high without worrying too much about doing something nasty to human biology. In other words, you can hit the virus really, really hard.
There’s a whole long happy tale of why Pfizer “just happened” to have an Mpro inhibitor lying around, involving work on the original SARS epidemic back in 2003. A good research lab never loses information! Knowledge always turns out to be good for something, and keeping the people around who can find it for you is a good idea.
The other component of paxlovid is ritonavir. This is a medication that’s been used in HIV and hepatitis C for years. Yes, it’s mildly a 3CLpro/Mpro inhibitor in its own right. But the main reason for it is that your liver, via a gene called CYP3A, will break down nirmatrelvir too fast! We’d practically have to keep you in the hospital with a continuous infusion to make nirmatrelvir work on its own.
Ritonavir to the rescue: it inhibits CYP3A, which makes nirmatrelvir stay active in your body longer, which means it can keep whacking on the virus longer. And it means we can send you home with a couple blister packs of pills instead of keeping you on an IV. On the (slight) downside, ritonavir is the reason why paxlovid interacts unfavorably with so many other drugs: they’re broken down by CYP3A also!
All very nice. A triumph of drug development, really, illustrating How It Is Done.
For Whom the Paxlovid Tolls… or Rather, “Works”
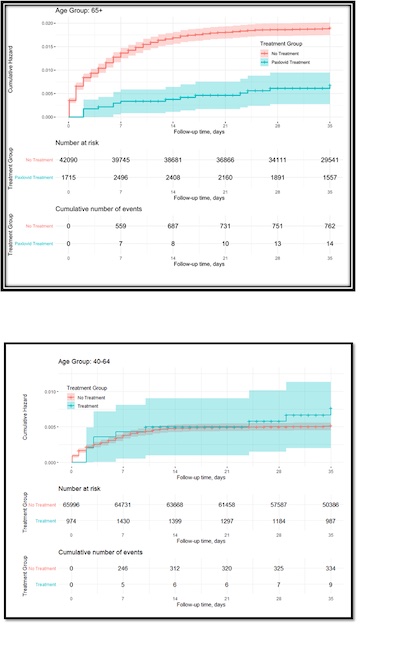 Previously on this CLBTNR we wrote about an Israeli study of where paxlovid has a huge
benefit and were it doesn’t.
[2] The conclusion we drew was:
Previously on this CLBTNR we wrote about an Israeli study of where paxlovid has a huge
benefit and were it doesn’t.
[2] The conclusion we drew was:
- For ages 65+: Paxlovid had a dramatic positive effect in reducing hospitalization and death rates.
- For ages 40-64: Paxlovid had not much effect at all on either hospitalization or death rates.
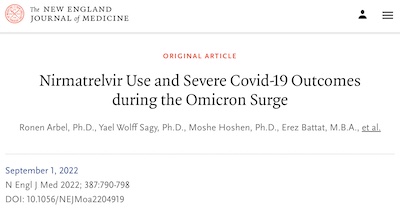 Now, that was based on a preprint, before peer review. So we were extremely pleased to
see that the paper held up under peer review and was published in the prestigious New
England Journal of Medicine last month. [3]
Now, that was based on a preprint, before peer review. So we were extremely pleased to
see that the paper held up under peer review and was published in the prestigious New
England Journal of Medicine last month. [3]
So kudos to the group at Clalit Health Services and Ben-Gurion University for some good, hard data on the merits of paxlovid. Solid work. Paxlovid is really, really good stuff. Also a great tale of effective drug discovery based on tons of past research. (Like the mRNA vaccines, for that matter, which are also based on decades of previous work!)
Why Don’t We See Much Effect for Ages 40-64?
Basically, paxlovid makes the response in elders more in line with the response in the middle-aged. It’s not that paxlovid doesn’t work for the middle aged, since it does shorten the time to healing. It’s just that the middle-aged have immune systems that are still pretty good and will probably recover without paxlovid. For the middle-aged, paxlovid just makes sure.
But for elders, with weaker immune systems, paxlovid fills a real gap in the risk, by fighting alongside their immune system to punch the virus hard enough that even an elderly immune system can cope.
The Weekend Conclusion
I think the conclusion still stands:
- Paxlovid is a big deal for people over 65. If you’re over 65 and get COVID-19, insist that your doc either write for paxlovid or present very specific medical reasons why not. (Usually drug interactions with other prescriptions which you cannot interrupt, even for 5 days.)
- For people under 65, it’s probably not a tragedy if you can’t get it. Probably. If I were still in that demographic, I’d still insist pretty hard until I got it prescribed, since it demonstrably does no harm and backstops your immune system. I mean, why take chances when theres’s (a) no reward for doing so and (b) the countermeasures are cheap, safe, and effective?
Paxlovid is good stuff. It’s woefully underprescribed, because of all the misinformation and press concentrating only on the very minor bad events.
Notes & References
1: Weekend Editor, “Med-Chem Optimization of Paxlovid”, Some Weekend Reading blog, 2022-Jan-19. ↩
2: Weekend Editor, “Paxlovid in the Wild”, Some Weekend Reading blog, 2022-Jun-02. ↩
3: R Arbel, et al., “Nirmatrelvir Use and Severe Covid-19 Outcomes during the Omicron Surge”, New Engl Jnl Med, 387:790-798, 2022-Sep-01. DOI: 10.1056/NEJMoa2204919. ↩
Gestae Commentaria
Comments for this post are closed pending repair of the comment system, but the Email/Twitter/Mastodon icons at page-top always work.