Nucleocapsid Abs & Severe COVID-19
Tagged:COVID
/
JournalClub
/
PharmaAndBiotech
/
SomebodyAskedMe
/
Statistics
Somebody asked me a couple months ago about the significance of high nucleocapsid antibodies in unvaccinated people compared to the vaccinated. Now there’s another paper exploring the meaning of N ab levels. Let’s see what it says!
The original question
A couple months ago, on behalf of a friend, we looked into nucleocapsid antibody levels and COVID-19 resistance. A friend of a friend noted higher N abs in unvaccinated people, and opined that unvaccinated people had more diverse antibody types, which might be protective over vaccination.
This was, of course, exactly backwards:
- Vaccinated people don’t bother making N abs because they don’t have to: their spike antibodies take care of the infection before it gets that far.
- Unvaccinated people make abs to everything SARS-CoV2 related, including the nucleocapsid protein, more or less in desperation to find something protective.
- The nucleocapsid protein is inside the viral envelope, so it’s useless: your immune system can’t see it until after it’s gotten inside a cell and opened up.
- The stats on infection rates in vaccinated vs unvaccinated populations are unequivocal: vaccination dramatically reduces the danger!
Association of Nucleocapsid Abs with Severe COVID-19
 So it was of great interest here at Chez Weekend, when a paper dropped last week, after
passing peer review, on the subject of nucleocapsid antibodies and COVID-19 severity.
[1]
So it was of great interest here at Chez Weekend, when a paper dropped last week, after
passing peer review, on the subject of nucleocapsid antibodies and COVID-19 severity.
[1]
First, a distinction: they measured N antigen levels, not antibody levels. That is, they looked at the viral protein levels themselves. The immune system forms antibodies in response to antigens, so this is kind of a proxy for antibody levels. (Or, maybe not: maybe high N antigens just mean high viral load, which would mean severe infection. Hard to say, but I lean toward the proxy-for-antibody levels interpretation.)
Study Design
Some background:
-
They measured $N = 2540$ subjects over a time window from 2020-Aug to 2021-Nov, in 114 centers across 10 countries. This is The Good Stuff, not a tiny, one-hospital study!
-
This is during the Delta wave, not the current Omicron.
-
Subjects were adults, hospitalized for COVID-19, with ≤ 12 days of symptoms. So the population is within a fairly narrow window of early/intermediate COVID-19.
-
They assessed via logistic regression – one of my favorite methods! – the association between binarized N antigen levels (< 1000 ng/l vs > 1000 ng/l) and a variety of clinical measurements, including:
- worsening on an ordinal pulmonary scale at day 5 (lungs getting worse fast), and
- time to hospital discharge.
They also used Fine-Gray regression models. I worked with Bob Gray on a project once, and was very impressed. Good guy.
So: good sized study, international in nature, well defined subject population, and good statistical method choices, and passed peer review!
Thumbs up, so far.
Some Results
The topline summary that they put in the abstract comes down to 3 things:
- Pulmonary severity strongly associated with antigen levels, 3.1 fold (CL: 2.22 - 4.34).
- Antigen stronger if no spike antibodies (unvaccinated), 6.42 fold (CL: 5.37 - 7.66).
- High antigen means with longer time to hospital discharge, 0.54 fold (CL: 0.45 - 0.57).
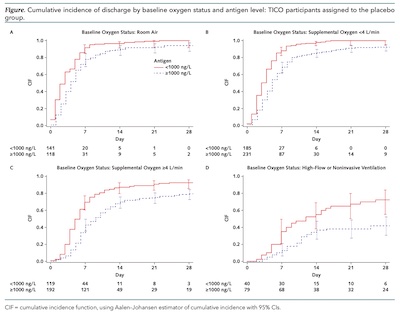 The main figure in the paper shows the hospitalization discharge rate graphically:
The main figure in the paper shows the hospitalization discharge rate graphically:
- The horizontal axis is time, in days since hospital admission.
- The vertical axis is the cumulative incidence fraction, i.e., what fraction of the patients have been discharged by a given day.
- The red solid curve is the low N antigen cohort (< 1000 ng/l), and the dotted blue curve is the high N antigen cohort (> 1000 ng/l).
- Each of the 4 panels shows the breakdown by oxygenation status: room air only, low O2 supplement, higher O2 supplement, and an even higher O2 status (but not intubated).
The figure highlights 2 conclusions, tested statistically elsewhere in the paper: low N antigen patients get discharged earlier, and that fact is true independent of oxygen treatment status.
As the authors put it:
Elevated plasma antigen is highly associated with both severity of pulmonary illness and clinically important patient outcomes. Multiple clinical and viral factors are associated with plasma antigen level at presentation. These data support a potential role of ongoing viral replication in the pathogenesis of SARS-CoV-2 in hospitalized patients.
The Weekend Conclusion
Basically, high nucleocapsid antigen levels are bad news. They leave in their wake high nucleocapsid antibodies, which is evidence of previous bad news.
So get vaccinated so you can avoid these bad things!
Notes & References
1: ACTIV-3/TICO Study Group, “The Association of Baseline Plasma SARS-CoV-2 Nucleocapsid Antigen Level and Outcomes in Patients Hospitalized With COVID-19”, Annals Int Med, 2022-Aug-30. DOI: 10.7326/M22-0924.↩
Gestae Commentaria
You might be interested in an article from the L.A. Times regarding an experimental vaccine that includes a second target for the nucleocapsid protein.
Oooh… that is interesting, thanks!
Of course having multiple targets is a well-known strategy for coping with resistance mutation. That’s one reason for combination therapies and multi-targeting antibodies in modern cancer therapy, for example.
I have a little trouble with the nucleocapsid protein as a target though: being inside the viral envelope, it’s only visible after infecting a cell.
Still, I’m eager to dive into the article and whatever papers are behind it. Thanks for the pointer.