US CDC ACIP Meeting: COVID-19 Vaccine Recommendations
Tagged:CatBlogging
/
COVID
/
JournalClub
/
MathInTheNews
/
PharmaAndBiotech
/
Politics
/
Statistics
Today the US Centers for Disease Control (CDC) Advisory Committee on Immunization Practices (ACIP) met, to decide recommendations on COVID-19 vaccines for 2024. Let’s go see what went down.
Agenda
The meeting is about several things, only one of which is COVID-19. I suppose that’s good news, of a sort, in that COVID-19 is now something we consider along with other medical problems instead of the world-ending disaster it might have been. This meeting also considers Chikungunya vaccines, diphtheria/tetanus vaccines, influenza vaccines, and polio vaccines.
 We’ll concentrate on just the COVID-19 part. The agenda for that is shown here
[1] in the morning, with voting to happen along with other
matters later in the day at 2pm.
We’ll concentrate on just the COVID-19 part. The agenda for that is shown here
[1] in the morning, with voting to happen along with other
matters later in the day at 2pm.
There’s even another part to the meeting tomorrow, though nothing COVID-19-related.
Looks pretty much like what you’d expect: some views on hospitalization and vaccine uptake rates, a review of efficacy and an economic (!) analysis, and then reasoning from evidence to recommendations.
Presentations
 Mostly we’ll rely on the presentations archived for the meeting, but occasionally today
we’ll check in on the BlueSky skeet thread of the redoubtable Helen Branswell of STAT
News [2], because she picks up a lot of detail and nuance,
and has been our trusted native guide in the past. Her main point so far is that there
are at least 6 vacancies on the ACIP that have not yet been filled, no idea why, so 6 CDC
folk will sit in as ex officio members on this meeting.
Mostly we’ll rely on the presentations archived for the meeting, but occasionally today
we’ll check in on the BlueSky skeet thread of the redoubtable Helen Branswell of STAT
News [2], because she picks up a lot of detail and nuance,
and has been our trusted native guide in the past. Her main point so far is that there
are at least 6 vacancies on the ACIP that have not yet been filled, no idea why, so 6 CDC
folk will sit in as ex officio members on this meeting.
I’m not going to watch the video and listen to the arguments, because that’s too much bandwidth for my Long COVID-19 befogged brain to handle. But I will go through each of the presentations, hunting for surprises.
Introduction to the Meeting
 As expected, there’s not much to report here. [3]
As expected, there’s not much to report here. [3]
It’s pretty much a summary of past meetings and recommendations for the Moderna, Pfizer, and Novavax vaccines. There’s a list of CDC personnel involved, as well as the voting meeting members.
The latter might be of interest if you’re trying to track member voting records to analyze for bias, otherwise this is pro forma and as expected.
(Beyond pro forma: Helen Branswell might point out that there are a lot of vacancies here, so the membership is CDC-heavy, with 11 CDC members and 2 outside advisors (slide 5). That… needs correction. Now.)
Hospital Surveillance
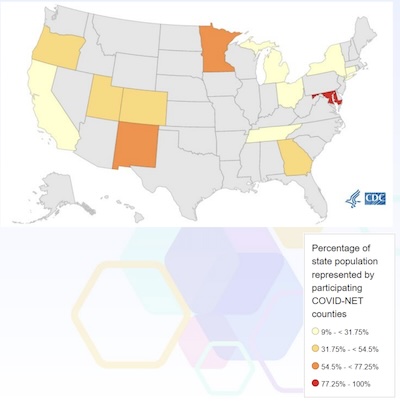 This is a COVID-19 hospitalization surveillance report from COVID-NET, a component of the
CDC RESP-Net program. [4] They have pretty broad coverage:
>300 acute-care hospitals in 98 counties in 13 states, 9/10 HHS regions. This reaches
about 10% of the US population. (High coverage in Maryland is understandable given that’s
where the CDC is. High coverage in New Mexico and Michigan are harder to explain?)
This is a COVID-19 hospitalization surveillance report from COVID-NET, a component of the
CDC RESP-Net program. [4] They have pretty broad coverage:
>300 acute-care hospitals in 98 counties in 13 states, 9/10 HHS regions. This reaches
about 10% of the US population. (High coverage in Maryland is understandable given that’s
where the CDC is. High coverage in New Mexico and Michigan are harder to explain?)
They’re looking at SARS-CoV-2 positive patients within 14 days or during hospitalization, as shown by screening or clinician-driven testing.
- Hospitalization rates break down along age groups as you’d expect, with the older clades being hospitalized more often.
- Current rates are about 40 per 100,000 among those over 75. Among those, about 25% were in long-term care facilities.
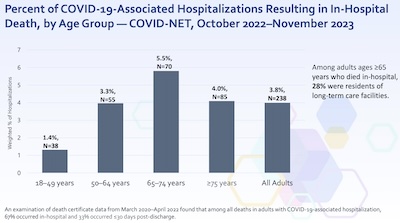
 Two other conclusions were pretty stark:
Two other conclusions were pretty stark:
- First, while the death rate of 1.4% at ages 18-49 sounds low, that’s still a lot of people. But the real point of this slide is that the death rate among elders is 5.5%. Basically, if you’re older and get hospitalized for COVID-19, 1 in 20 of you will die. This is amazingly high, and should prompt a relentless vaccination education program for elders, particularly those in long-term care.
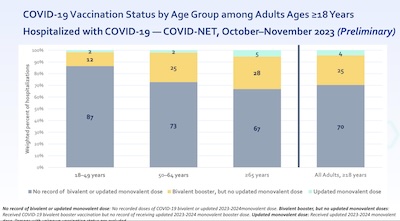
- Second, the overwhelming majority of those hospitalized are unvaccinated (or for whom
there is no record of vaccination). At this point, remaining unvaccinated is just a
death wish, and we desperately need to educate elders about this to get them
vaccinated.
- NB: There is a nuance here, since we’re observing that $\Pr(\mathrm{Unvaccinated} | \mathrm{Hospitalized})$ is high, since we’re looking only at the hospitalized population.
- The real risk of course is the Bayesian dual, $\Pr(\mathrm{Hospitalized} | \mathrm{Unvaccinated})$ to uncover the real risks of remaining unvaccinated. When we’ve examined that before on this Crummy Little Blog That Nobody Reads (CLBTNR), it’s been utterly damning: remaining unvaccinated dramatically shortens lives.
Vaccine Coverage
 Next, on to vaccine coverage. [5] This, alas, is some pretty
concerning stuff!
Next, on to vaccine coverage. [5] This, alas, is some pretty
concerning stuff!
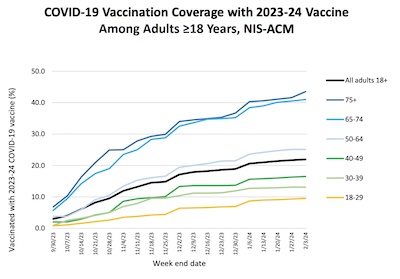
- As shown in the graph here from slide 3, uptake of the 2023-2024 booster from last fall
has been (a) low, (b) slow, and (c) stratified by age:
- The plateau is only 40% uptake, and that’s among elders who received the most benefit. Why not more of them? No idea, here.
- It took almost 3 months to reach the apparently-final plateau. Why did people take so long to make such an obvious decision? No idea, here.
- In some ways worst of all, the uptake curves stratify by age. Younger people took up
the booster at measly rates of 5% – 20%. This means they get sick, again and
again, accumulating damage and risks of Long COVID. They also become carriers who
force the elders with whom the come in contact to be exposed to potentially lethal
risks (“granny-killer” is the derisive, but apt, term). Why such contempt for their
own future health and that of their elders? No idea, here.
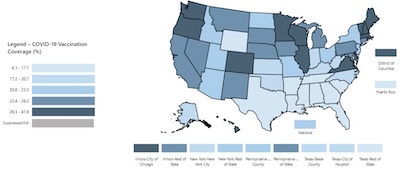
- Ok, so who are these people stubbornly refusing a booster? We see the geographic
distribution on slide 4, shown here. As you can see, the concentration is miserably
high in the American South, and some Midwestern states.
- These are the red/Trumpy states that resist not just vaccines, but science education in general, want to whitewash their complicity in slavery in the Civil War, criminalize women’s health care, and lots of other barbarisms.
- We’ve previously documented the undeniable relationship between county-level Trump
voting rates and vaccine resistance rates. The only consolation there is a dark one:
this is evolution in action, where stupidity is given capital punishment.
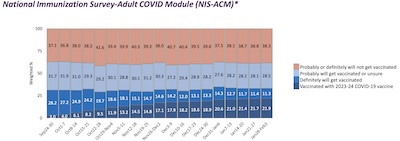
- Is this a new thing? Alas, no, as shown by this plot on slide 5. It’s from a survey of
$N = 257,352$ people, asking about their intentions to get a booster (or a vaccine at
all).
- We see, sustained over time the last 6 months, that there is a steady cohort of people who absolutely refuse vaccination (about 40%) and another cohort that is wishy-washy or somehow “unsure” (about 30%).
- That means 60% – 70% of people behave recklessly enough to explain why we have low
vaccine uptake numbers that endanger all of us.
- Ok… sigh: it’s largely a Southern/Midwestern/Trumpy thing, and it persists over time.
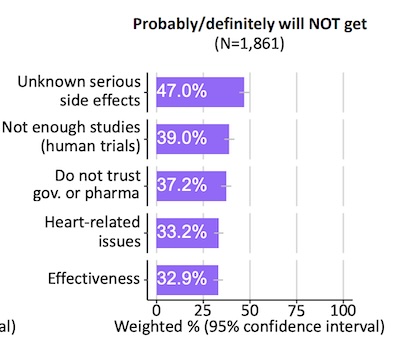
What can they possibly be afraid of this time? Consider this extract from slide 11,
detailing the frightening canards:
- They fear “unknown” side-effects in a medication that has had billions of doses given. I’m not sure how anything can be an unknown side effect at this point, but rationality isn’t what’s going on here.
- They still think not enough human trials have been done… in spite of the largest Phase IV trial in human history, where billions of people have been vaccinated. This is pure hallucination.
- They “don’t trust” government or pharma companies. I get it, but I don’t get why they want to die for this paranoia.
- They think the relatively rare cardiac inflammation is way more common, in spite of ample statistical evidence to the contrary.
- And, of course, they think the vaccines don’t work. I can’t even begin to
understand the utter bone-headed hopelessness of this view.
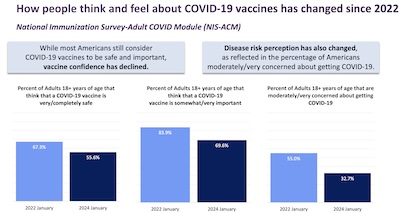
- Has it been getting worse? Sadly, yes, according to the analysis from slide 17 shown
here.
- Confidence in vaccines has declined over the last 2 years, despite the overwhelming success of the mRNA vaccines in particular.
- In parallel, people have become quite blasé about the importance of vaccination
and the risks of getting COVID-19. This in spite of the increasing evidence of the
accumulation of risk of Long COVID-19 with each infection.
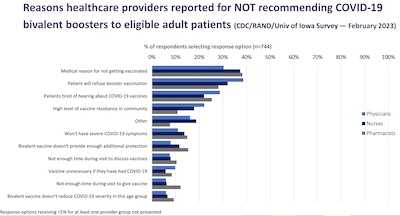
- Ok, what about health care providers? Surely they, as people educated in these matters, must be giving better reasons? Again alas, no, not according to the data presented on slide 22. The list of reasons why HCP’s sometimes don’t recommend vaccination (which can occasionally be the right thing) are in fact pretty silly. They include fear a patient would refuse, patients being “tired of hearing about COVID-19”, community vaccine resistance, thinking vaccines aren’t protective enough, just no time in a visit to discuss or give a vaccine (thanks, insurance executive MBA’s!), and so on.
Can you tell I’m incandescently angry about our low vaccine uptake?
Public health is not a matter of personal responsibility! Public health is a public matter, in which we must be responsible for each other by practicing good preventive medicine for ourselves and others.
Thinking only of public health as a personal responsibility is a sociopathic level of self-regard.
Nevertheless, here we are.
Vaccine Efficacy
 So vaccine coverage is pretty miserable; we’re just not vaccinating enough people and the
reasons given are delusional.
So vaccine coverage is pretty miserable; we’re just not vaccinating enough people and the
reasons given are delusional.
How about vaccine efficacy? Maybe the vaccines are so good that it won’t matter?
Dream on, alas. The report on vaccine efficacy [6] tells us the news. Not exactly bad news, but at best mediocre.
She starts out wisely by reviewing the definition of efficacy and debunking some of the bonehead misconceptions about it. If $p_v$ is the probability of getting infected, hospitalized, or dead in the vaccinated population, and $p_c$ is the similar probability in the control population, then vaccine efficacy is:
\[VE = 100\% \times \frac{p_c - p_v}{p_c} = 100\% \times \left(1 - \frac{p_v}{p_c}\right)\]That is, how much does vaccination lower the chance of getting infected, hospitalized, or dead, expressed as a percent of the baseline rate $p_c$?
It strongly depends on the outcome measure (infected at all, hospitalized with serious disease, or death). It also depends on the control group: totally unvaccinated people, people with another vaccine, people with the previous vaccine but without a booster, etc.
We should expect the number to change, since the background population has changed since 2020. We should also expect it to change since sensitivity and specificity of testing has changed, too.
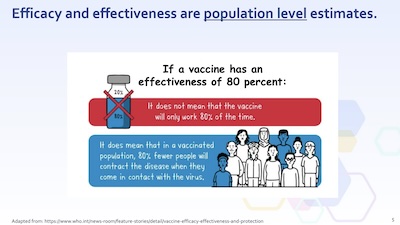 She then — admirably, in my view — addresses some of the public’s
misconceptions about vaccines. The problem with any sentence involving the word
“probability” is that the public will replace that with “opinion” or “can be ignored for
now”. Here on slide 5 she points out that “80% efficacy” does not mean the vaccine only
works 80% of the time; it is a population level statement about lowering your risk by 80%.
She then — admirably, in my view — addresses some of the public’s
misconceptions about vaccines. The problem with any sentence involving the word
“probability” is that the public will replace that with “opinion” or “can be ignored for
now”. Here on slide 5 she points out that “80% efficacy” does not mean the vaccine only
works 80% of the time; it is a population level statement about lowering your risk by 80%.
Once again, public health is a public matter, requiring collective action, not just individual responsibility. It’s good to remember that these committee meetings and their public archives are meant to address the public, as well as professionals.
Here we’re comparing those getting the updated 2023 – 2024 booster vs those who were eligible for it but did not receive it. That control group has considerable built-in immunity due to previous vaccinations and previous infections, so we should expect efficacy lower than the initial 95% in 2020 (compared to a then-naïve population).
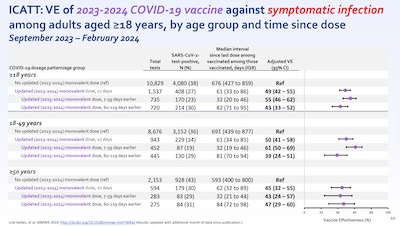 She looks at this multiple different ways (symptomatic infection vs hospitalization,
measuring infection by antigen test vs more sensitive tests, and stratifying by age).
That’s admirable, but we can summarize: all of them give results around 50% efficacy,
i.e., the booster reduces risk by about 50%.
She looks at this multiple different ways (symptomatic infection vs hospitalization,
measuring infection by antigen test vs more sensitive tests, and stratifying by age).
That’s admirable, but we can summarize: all of them give results around 50% efficacy,
i.e., the booster reduces risk by about 50%.
Slide 10 shows this, for symptomatic infection, stratified by age and by time since boosting. All the results are around 50%, with error bars going from 30% to 70%. Other slides look at other outcomes and other test methods, but all say around 50% risk reduction.
Keep in mind, that’s a 50% reduction in risk, on top of the immunity already present in our population with a high rate of previous infection and reasonable (though not high enough) rate of vaccination. Still pretty good!
Economics of an Additional Dose for Elders
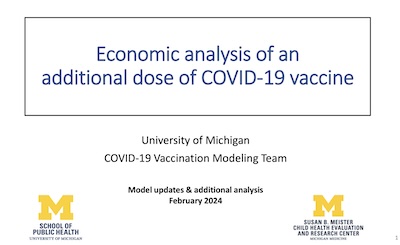 Next up was an economic analysis of giving additional doses to the
elderly. [7]
Next up was an economic analysis of giving additional doses to the
elderly. [7]
I have to be honest: I hate this sort of thinking.
- First, there is a great deal more to life than economics. If you let economics be your guide in all things, you’ve assumed a simpler utility function than I’d prefer. The downside of that is the inevitability of utility monsters, i.e., being forced into cruel behavior to those with little money or power. (This is the source of so much cruelty in libertarianism that makes me hold it in complete contempt.)
- Second, I used to hear this sort of argument in the workplace every couple months about mental health research. It always went something like: depression costs us this many billions in lost work hours, so we should do research on treating it. Really? Work hours are the most important thing here? The fact that depression makes people miserable and kills many is not enough?
And so it is here. Boosters save lives. Shouldn’t that be enough?
But as it is for many people not enough… here we are.
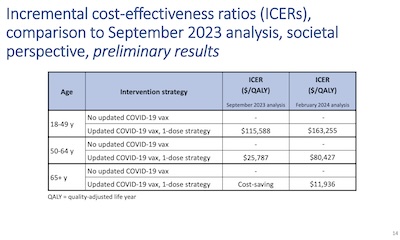 I won’t go through their analysis, because it was hard enough to stop the gorge rising the
first time through. But here’s their result, on slide 14.
I won’t go through their analysis, because it was hard enough to stop the gorge rising the
first time through. But here’s their result, on slide 14.
- They’re measuring the cost in $/QALY (quality-adjusted life year, sort of medical calculation including number of years of life extension and the quality of life for those years).
- The outcome says you make a “profit” in doing this for seniors, but not others. (Those lives are too expensive to save, apparently.)
(The analysis was done multiple ways, looking at 1-dose vs 2-dose strategies and measuring various outputs, but the results indicated a similar outcome.)
Evidence to Recommendation Analysis of Additional Dose for Elders
 Ok, enough with the economic analysis. The FDA and CDC have a formal process in place for
this, called Evidence to Recommendations, or E2R. It’s supposed to be a transparent way
of reasoning from what we see in nature to what we should do about it, policy-wise. I’m
sure it’s a nightmare in some ways, but it at least covers some of the cases previously
seen, so let’s at least try it.
Ok, enough with the economic analysis. The FDA and CDC have a formal process in place for
this, called Evidence to Recommendations, or E2R. It’s supposed to be a transparent way
of reasoning from what we see in nature to what we should do about it, policy-wise. I’m
sure it’s a nightmare in some ways, but it at least covers some of the cases previously
seen, so let’s at least try it.
That’s the thrust of the next presentation: what does E2R say we should do? [8]
They go through about the sorts of things you’d expect:
- history of previous vaccinations,
- the response in terms of hospitalization & death rate decreases,
- seroprevalence of SARS-CoV2 stratified by infection history and age,
- the immunology of aging,
- whether the policy will have equitable impact,
- rates of waning of vaccine-induced immunity,
- vaccine safety in the affected groups,
… and so on. There’s a lot of stuff here.
I wasn’t able to discern any mathematics in the E2R work, as apparently it’s a way of structuring arguments in the CDC committees. But… it came out the same as above, that seniors should get a booster.
Next Steps in the Vaccine Program
 Finally, they took a look forward at what vaccine policy should be in the future and what
strains should be included. [9]
Finally, they took a look forward at what vaccine policy should be in the future and what
strains should be included. [9]
One big item was basically how to move faster! Last year, we settled on the BA.2.86 strain with glacial slowness; consequently we’re now using a vaccine based on BA.2.86 while the current dominant strain is JN.1. Yes, there’s some cross-reactivity, but not as much as we’d like and it won’t necessarily be that way next time. So there was some critical review of the timelines from last year.
The annual flu vaccine manages to do this, as we’ve pointed out numerous times previously. Now perhaps the CDC will put the COVID-19 timelines on a similar scale, and hope for a similar result.
And… that’s basically it. No discussion of future multivalent strains, or rapid response of changing vaccine strains.
A bit disappointing, but at least they acknowledge they’ve been too slow in the past.
Voting Results
For this section, I watched live. Started at 2:06pm, only 6min late, which is kind of impressive, as these things go!
Voting proposition: “ACIP recommends that persons ≥65 years of age should receive an additional dose of 2023-2024 formula COVID-19 vaccine.”
- Discussion point: 40% of elders don’t have even the first shot, so improve that too. Also, dosing later than June if there’s a new formulation this fall is suboptimal, so do it soon if at all.
- Votes: Yes: 11, No: 1, Abstain: 1. All voters reported “no conflicts”, i.e., not employed by or heavy stock ownership in a vaccine provider. (On some of the other non-COVID-19 votes, a few members had conflicts, declared them, and recused themselves.) No discussion about the no vote or the abstention vote.
So: by a vote of 11-1-1, the recommendation of a spring booster passed.
 The venerable Globe reported this result the same evening. [10]
They emphasized that COVID-19 is not seasonal, so there’s year-round risk. Boosts in
the elderly tend to wear off in about 180 days, so twice-yearly boosting just makes
sense. The initial language saying this group “may” receive a booster was promoted to
“should”, because why be wishy-washy when people will just use that as an excuse not to
listen? Still, vaccine booster uptake remains disappointingly low.
The venerable Globe reported this result the same evening. [10]
They emphasized that COVID-19 is not seasonal, so there’s year-round risk. Boosts in
the elderly tend to wear off in about 180 days, so twice-yearly boosting just makes
sense. The initial language saying this group “may” receive a booster was promoted to
“should”, because why be wishy-washy when people will just use that as an excuse not to
listen? Still, vaccine booster uptake remains disappointingly low.
Now, how soon can I call my local pharmacy and expect them to have a clue what I’m talking about? I bet it’ll take at least a week to percolate through insurance, PBMs, and corporate bureaucracy.
Vaccine Composition Going Forward
 So what about vaccine strains going forward, for this fast-evolving virus?
So what about vaccine strains going forward, for this fast-evolving virus?
The FDA’s Vaccines and Related Biological Products Advisory Committee (VRBPAC) meets on 2024-May-16 to decide exactly that. [11] All we know for now is that that’s the agenda:
Agenda
On May 16, 2024, the Committee will meet in open session to discuss and make recommendations on the selection of strain(s) to be included in the 2024-2025 Formula for COVID-19 vaccines. The meeting presentations will be heard, viewed, captioned, and recorded through an online teleconferencing and/or video conferencing platform.
The CDC’s ACIP promises to meet in June to review previous results and bless (or not) the new mix proposed by the FDA’s VRBPAC.
The Weekend Conclusion
That’s… more or less as expected?
The Weekend Publisher and the Assistant Weekend Publisher, shown here in their top management executive chair, agree that this is what they expected.
It seems quite obvious – though here we are, a posteriori, where it darn well should be obvious – that since immunity fades quickest in elders and hospitalization is most likely lethal in elders, a boost for elders is sensible.
So why do these committee meetings always seem to take the long way ‘round to reach a conclusion that’s sitting right there in front of them? Before you resort to the “government bureaucracy” slur, consider that they might be practicing “defensive medicine”, i.e., carefully documenting each decision to avoid it being used against them (and against public health).
They’re just as aware as the rest of us, and probably more so, of the delusional conspiracy thinkers who hallucinate various threats around vaccines. By doing things this way, they can just point people to the public meeting record to show they’ve done the required work, and done so transparently.
They’ve dotted all the i’s, crossed all the t’s, and… for all I know, checked every umlaut for bööby traps. You can’t credibly accuse CDC/ACIP of taking shortcuts, or that not enough trials have been done, or not enough side effects have been considered, as the crackpots were shown to believe above. (But you can credibly identify crackpots, when they utter such arguments.)
Yes, that’s sad. Also, surprising: I would not have thought pre-pandemic that we’d be dense as a sack of bricks. But, as all the existentialists say, here we are.
So go get boosted if you’re old enough.
(Ceterum censeo, Trump incarcerandam esse.)
Notes & References
1: CDC ACIP Staff, “Final February 26, 2024 Agenda: MEETING OF THE ADVISORY COMMITTEE ON IMMUNIZATION PRACTICES (ACIP)”, CDC web site, 2024-Feb-28. Links to presentations on the associated web page. ↩
2: H Branswell, “BlueSky thread on ACIPmeeting”, BlueSky account of Helen Branswell of STAT News, 2024-Feb-28.↩
3: MF Daley, “Introduction: ACIP COVID-19 Vaccines Work Group”, CDC web site, National Center for Immunization and Respiratory Diseases, 2024-Feb-28. ↩
4: CA Taylor, “COVID-19–Associated Hospitalizations among Adults — COVID-NET, 2023–2024”, CDC web site, RESP-NET Hospitalization Surveillance Team, 2024-Feb-28. ↩
5: K Chatham-Stephens, “An update on COVID-19 vaccination coverage”, CDC web site, National Center for Immunizations and Respiratory Diseases (NCIRD), 2024-Feb-28. ↩
6: R Link-Gelles, “Vaccine effectiveness of updated (2023-2024) COVID-19 vaccines”, CDC web site, Coronavirus and Other Respiratory Viruses Division of US Public Health Service, 2024-Feb-28. ↩
7: University of Michigan COVID-19 Vaccination Modeling Team, “Economic analysis of an additional dose of COVID-19 vaccine”, CDC Web site, UMich School of Public Health & Susan B Meister Child Health and Evaluation Center, 2024-Feb-28. ↩
8: M Wallace, “Evidence to Recommendations Framework: Additional Dose of 2023-2024 Formula COVID-19 Vaccine in Older Adults”, CDC web site, National Center for Immunization and Respiratory Diseases, 2024-Feb-28. ↩
9: L Panagiotakopoulos, “Next Steps for the COVID-19 Vaccine Program”, CDC web site, National Center for Immunization and Respiratory Diseases, 2024-Feb-28. ↩
10: A Piore, “CDC recommends additional COVID-19 booster for people over age 65”, Boston Globe, 2024-Feb-28. ↩
11: FDA VRBPAC Staff, “Vaccines and Related Biological Products Advisory Committee May 16, 2024 Meeting Announcement”, FDA Advisory Committee Calendar web page, 2024-Feb-28. ↩

Gestae Commentaria
Comments for this post are closed pending repair of the comment system, but the Email/Twitter/Mastodon icons at page-top always work.